The healthcare industry has become a key area of economic activity. It is being rapidly privatized, with deeply negative results, except for the happy few at the top of the wealth pyramid. Free unfettered market can work best for your choice of shoes. But for healthcare, it is a disaster. It is not a question of ideology, but of looking at the examples of what works best.
(Ladislau Dowbor)
Far from providing Universal Health Care, the legacy of development finance institutions’ investments in for-profit private healthcare is more likely to result in a growing concentration of wealth and power in the hands of a small number of incredibly wealthy men.1
Ideological simplifications in economics are a curse, and they are based not only on ignorance, but basically on financial interest. Paxlovid, a recent Pfizer 5-day treatment for Covid, with 30 pills, is being sold at US$1,390, while Harvard researchers found that the production cost for the full treatment is on the order of US$13. How far can this absurdity go? The key issue here, is that decisions are made not on how much health improvement you can provide, but how much money you can extract, even if you drastically reduce accessibility. For the algorithms calculating the marketing optimization, it is obvious that in the rich community clients will not see much difference between 100 and 1000 dollars, if they feel threatened – they are very sensitive – and will pay any price. The algorithms will reflect the logic that was built in it: maximize returns. The ideology gives the righteous feeling support: maximizing money is right, and is the moral of this sport.
The justification could be that they had to spend a lot on research. This is partly true, of course, and it is valid for several of the Big Pharma corporations. But the truth is that the huge progress we have made in health research is distributed around the world, and is mostly inherited from the overall scientific advances that gave us the understanding of DNA, the electronic microscopy, bioinformatics, AI, nanotechnology and so many structural transformations in the technological basics of research. If a corporation has an end-product, for which the population will have to pay, while most of the research-capacity inputs have been inherited, and paid by our taxes, it represents, as Gar Alperovitz and Lew Daly called it, “unjust deserts”.
The OxyContin scheme brings us another dimension, where causing deaths on a large scale is irrelevant, as long as it pays. The opioid crisis “evolved from prescription pills to illicitly-produced fentanyl and other drugs that together have claimed 800,000 American lives over the past quarter of a century with predictions of another million deaths by the end of the decade.” The Sackler family, Purdue and Johnson&Johnson were brought to justice, but resulting in just a few fines: “Federal regulators and prosecutors failed to seize the moment. Again, big pharma slipped away. Prosecutors negotiated a deal in which Purdue paid a large fine but was allowed to go on selling OxyContin largely unfettered, and a deal was struck for its executives to plead guilty to misdemeanors and avoided prison time…The US is still failing to learn the lessons of a uniquely American catastrophe to break the influence of corporate money over medicine, drug regulation and political accountability.” 2
We can find thousands of examples of fraud, marketing lies and other illegalities. You can just search on the internet, placing the name of any Big Pharma corporation together with “settlements”. The logic is simple: it is a different area of legal responsibility, where the culprits pay huge sums, but still peanuts compared to their profits, and are free not only from jail, but from admitting guilt. Wikipedia also provides a “list of largest pharmaceutical settlements”, each in the billions of dollars, for False Claims Act violations and the like. Snake-oil was childish game in comparison. It is done with armies of lawyers, top-notch specialists in business, finance, and even drugs. It is not a question of not knowing what they are doing. And they interrupt your TV program for a cute lass saying how marvelous this medicine will be for you. You pay for this commercial, its cost is included in the price of the products. Some 27% of the price of a Johnson&Johnson product is for marketing costs, not for research.
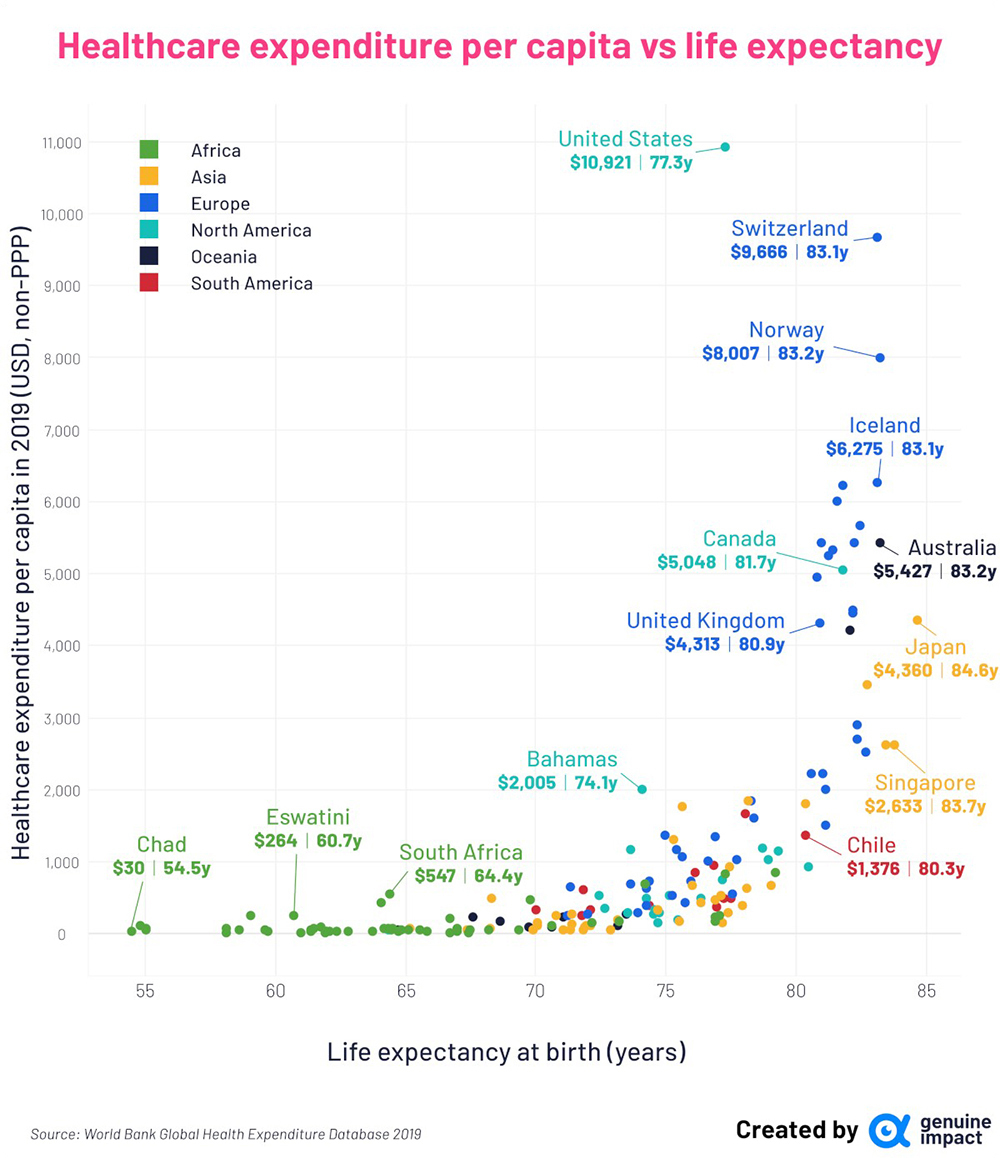 Source: Charted: Healthcare Spending and Life Expectancy, by Country.
Source: Charted: Healthcare Spending and Life Expectancy, by Country.
These few examples concern Big Pharma, but a similar logic applies to so many privatized health services. The question we raise here, is whether privatization is compatible with building healthy lives, not just making money on health services. The basic issue is that a privatized health system, with public regulation support, which is the US model, is a systemic failure. It is incompetent and inefficient. In Brazil, as in the US and other countries, the concentrated powerful health corporations have taken over the regulation institutions. The claim is often that “self-regulation” is sufficient. But it is a disaster.
The numbers are very explicit in the figure above. Healthcare expenditure in the US, in 2019, was US$10,921 per capita, and life expectancy 77.3 years. It is the basically privatized and unregulated system we have seen. In Canada, where healthcare is basically public, free and with universal access, the per capita cost was US$5,048, less than half, and life expectancy 81.7 years. The logic is not complicated: where you organize healthcare to maximize the population’s health, you will concentrate, among others, on preventive health, on clean water, on emissions control, on vaccine, on healthier cities, instead of concentrating on selling as much medicine and curative services as possible. It is about health, not business.
This World Bank study is sobering. In the UK, the corresponding figures are US$4,313 and 80.9 years, despite so many attacks on the NHS. Denmark is another interesting case of basically public health service, US$6,003 and 82 years. In France, US$4,492, and 82 years. On another level, Cuba is an interesting example, with US$1,032 expenditure and 79 years, higher than the US 77 years. For Brazil, the figures are US$853, and a life expectancy of 76, thanks in great measure to the public SUS system. The Brazilian health insurance groups, [planos de saúde], in part owned by US private health corporations like United Health, or the asset management industry like BlackRock, are an impressive example of systemic inefficiency. They drain financial resources of roughly 50 million people. When you retire, you won’t be able to pay for it anymore, in an age where you would most need it.
Private health services have become a huge financial arena. Overall, health services represent almost 20% of GDP in the US, it is its biggest industry, with dramatically poor results, unless you are in the rich club with access to private luxury health-service islands. “Meanwhile, a third of uninsured Americans cannot afford to take their medication, and almost half of those who are not covered by insurance asked their doctors for cheaper options. House Speaker Nancy Pelosi (D-Calif.) unveiled her party’s plan last week to give the government a say in prescription drug price-setting. Dubbed the Lower Drug Costs Now Act.”3 They are still fighting.
What is impressive is that the US offer the most inefficient and costly model, but this is the model gradually being expanded in many countries, because it pays, even if it leaves most of the population in dramatic situations. The reason is that it is part of a global financial integrated system. I pay a housekeeper a day a week for cleaning in my home in São Paulo. She has health problems, so she got into a private health insurance group, called Notre Dame. I checked data on this corporation, and found, among its investors, BlackRock. So, a part of what I pay to a modest person in Brazil is transferred to international shareholders, in fractions of a second, as virtual money. This capillarity of financial drains with virtual money works on a world scale. We need health, and in desperate situation we pay anything, and get in debt, or delay seeking care until things get worse, and more expensive. It is an overall flawed management system.
There is an obvious ethical dimension. Making access to healthcare more difficult, to make more money, is simply immoral. And you make more money with serving the wealthy. So many dramas in a rich country like the US is simply absurd. What do the asset management giants know about health services, except how much money they can extract? But the economic dimension is equally absurd. And it is about basic economics: with many producers and a richeness of choice, competition can stimulate better products and prices. Not in the case of the healthcare system.
A person facing a health problem is not chosing, he or she will follow instructions. The information inequality is radical. A friendly doctor put it straight to me: he works in a private hospital, and has to fulfill quotas of procedures, which the hospital will charge the health insurance, which in turn makes approval of procedures difficult, demanding case by case approval. The health insurance group will charge as much as possible from the public, charging for coverage: the health insurance group is usually linked to an asset management giant, and shareholder value is central. In the triangle between the doctor, the hospital and the health insurance interests, the patient’s interests come last. It is costly and inefficient, and does raise GDP, but what we need is more health, better and cheaper services. When you raise costs and prices, you do rise GDP, but the wrong way.
The basic idea I am trying to convey here, is that some activities clearly work better in a free-market environment, like producing bicycles, tomatoes, or opening a bar. But putting our health in the hands of financial corporations in a profit maximization environment, is just a tribute to incompetence. And the resulting deaths and suffering are dramatic, not to speak of the permanent feeling of insecurity, for ourselves or for our families. It is just a question of following the proven examples of what works best: universal public free access. How long will Americans be crossing the border to Canada?
References
1 Private health companies prosper while healthcare access stagnates, Peoples Health Dispatch, 2023.
2 ‘I don’t see how it ends’: expert sounds alarm on new wave of US opioids crisis, Chris McGreal, 2024.
3 Big Pharma Invests Millions as Congress Prepares Drug Pricing Bills, Yue Stella Yu, 2019.















